Indicators Of Metachromatic Leukodystrophy
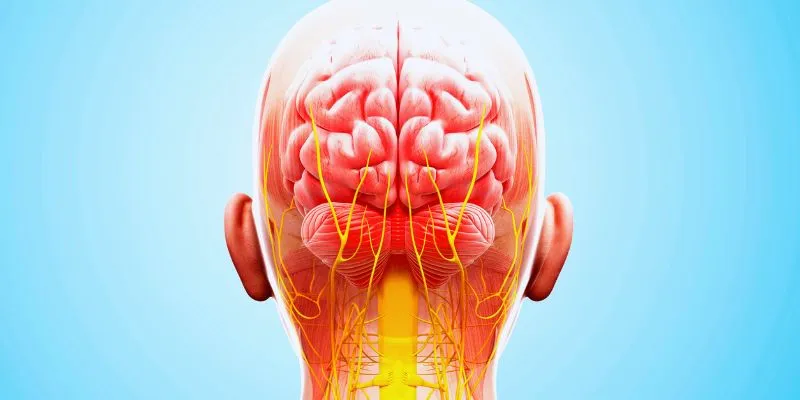
Metachromatic leukodystrophy (MLD) is a rare and progressive hereditary condition affecting the neurological system. It results from the accumulation of sulfatides, a type of fat, which damages the myelin sheath surrounding nerve cells. Children are primarily affected by this condition, leading to various psychological and physical challenges.
Recognizing MLD’s symptoms early can significantly help in managing the condition and providing timely interventions. This article explores the common signs of Metachromatic Leukodystrophy, offering guidance for concerned parents and caregivers on recognizing the early symptoms and diagnosis of MLD.
Early Signs of Metachromatic Leukodystrophy in Children
While each child may exhibit different symptoms of metachromatic leukodystrophy, there are several common early signs parents should be aware of. One of the earliest noticeable symptoms is a delay in developmental milestones. A child might find it difficult to sit, crawl, or walk at the expected age. Although these delays might appear minor initially, they typically worsen as the disease progresses. Behavioral changes are another early indication of MLD.
Young children may become unusually restless, less responsive, or withdrawn. Although these behaviors might sometimes be mistaken for typical toddler behavior, worsening symptoms could signal a more serious issue. Some children may also face challenges with motor coordination, experiencing difficulties in walking, balancing, or grasping objects. Identifying these early motor skill challenges is crucial for obtaining a proper diagnosis and initiating treatment to slow the disease’s progression.
Motor and Cognitive Decline in Metachromatic Leukodystrophy
As Metachromatic Leukodystrophy progresses, children’s physical and cognitive abilities decline significantly. Motor decline is characterized by reduced muscle strength and coordination. Children who could walk may eventually lose this ability, requiring wheelchairs for mobility, and may experience increased muscle spasms and stiffness. Physical therapy and supportive care are essential for managing these symptoms and helping children maintain some level of independence.
Cognitive decline often parallels physical changes. Children with MLD may regress in social skills, communication, and learning. They might struggle with understanding or speaking language. Cognitive abilities, such as memory, problem-solving, and recall, also diminish. This can be distressing for families as the child becomes unable to engage in previously enjoyed activities. To detect MLD early and initiate appropriate treatments, a pediatric neurologist may conduct various tests to monitor both motor and cognitive functions.
Behavioral Changes and Emotional Impact of MLD
Children with Metachromatic Leukodystrophy can exhibit behavioral changes ranging from emotional distress to irritability and mood swings. These changes are primarily related to the loss of cognitive abilities and the physical challenges associated with MLD. Children may become more prone to temper tantrums, aggression, or outbursts, which can be challenging for parents to manage. Occasionally, children may also undergo personality changes, withdrawing from social interactions or showing less interest in activities they once enjoyed.
Emotional disengagement can lead to increased isolation, complicating the family’s ability to cope with the disease’s progression. Both the child and family experience significant emotional strain. Support from counselors and specialized care professionals is vital in helping families navigate these challenges. Managing the behavioral aspects of MLD requires a comprehensive approach, including therapy, counseling, and sometimes medication.

Sensory and Visual Changes in MLD
Sensory alterations provide another critical clue of metachromatic leukodystrophy. As the disease progresses, children may experience difficulties with vision and hearing. Vision loss is the most common sensory change, with children struggling with visual coordination skills, such as reading, writing, or recognizing faces. They might also display signs of vision impairment, like squinting or covering one eye to see more clearly.
In some cases, as the disease progresses, a child may become blind or severely visually impaired. Although less common than vision issues, hearing loss is another concern. Children might struggle to respond to sounds or fail to react when their names are called. If sensory problems are noticed, it’s crucial to consult an ophthalmologist or audiologist to assess the level of impairment and develop a plan for appropriate interventions.
Diagnostic Approach to Metachromatic Leukodystrophy
Diagnosing metachromatic leukodystrophy involves a combination of imaging exams, biochemical tests, and genetic analysis. Typically, the process begins with a comprehensive clinical examination. A clinician will look for common indicators like developmental delays, motor coordination issues, and cognitive regression.
Genetic testing plays a significant role in diagnosing MLD. Testing the ARSA gene is essential in confirming the diagnosis, as mutations in this gene cause metachromatic leukodystrophy. Additional evidence of the condition comes from biochemical tests that measure sulfatide levels in plasma or urine. Damage to the brain’s white matter, characteristic of MLD, can be detected through advanced imaging techniques like magnetic resonance imaging (MRI). Early and accurate diagnosis is crucial for determining the most effective treatment plan. While there is no cure for MLD, early intervention can help improve the quality of life for affected children.
The Importance of Early Diagnosis and Intervention
Timely diagnosis and intervention are vital in managing metachromatic leukodystrophy. Early detection of MLD can delay disease progression and improve symptom management. With early diagnosis, children can benefit from therapies aimed at improving motor skills, coordination, and cognitive deficits, including physical, occupational, and speech therapy.
Genetic counseling is another crucial component of early intervention. Families with a history of MLD can seek genetic counseling to better understand the risk of passing the disease to future generations, as MLD is hereditary. Support groups and resources for families provide both emotional and practical assistance during this challenging time. Although there is no known cure for MLD, treatment focuses on symptom management, and ongoing research into potential therapies offers hope for future advancements in treatment.
Conclusion
Recognizing the signs of Metachromatic Leukodystrophy (MLD) is essential for early intervention and treatment. Early indicators often include cognitive regression, motor difficulties, and developmental delays. Additionally, behavioral, sensory, and emotional changes signal the progression of the disease. Early diagnosis, facilitated by genetic and biochemical testing, can lead to a better quality of life and effective management for affected children. While MLD cannot be cured, timely support, therapy, and family counseling are crucial in managing this rare condition.











